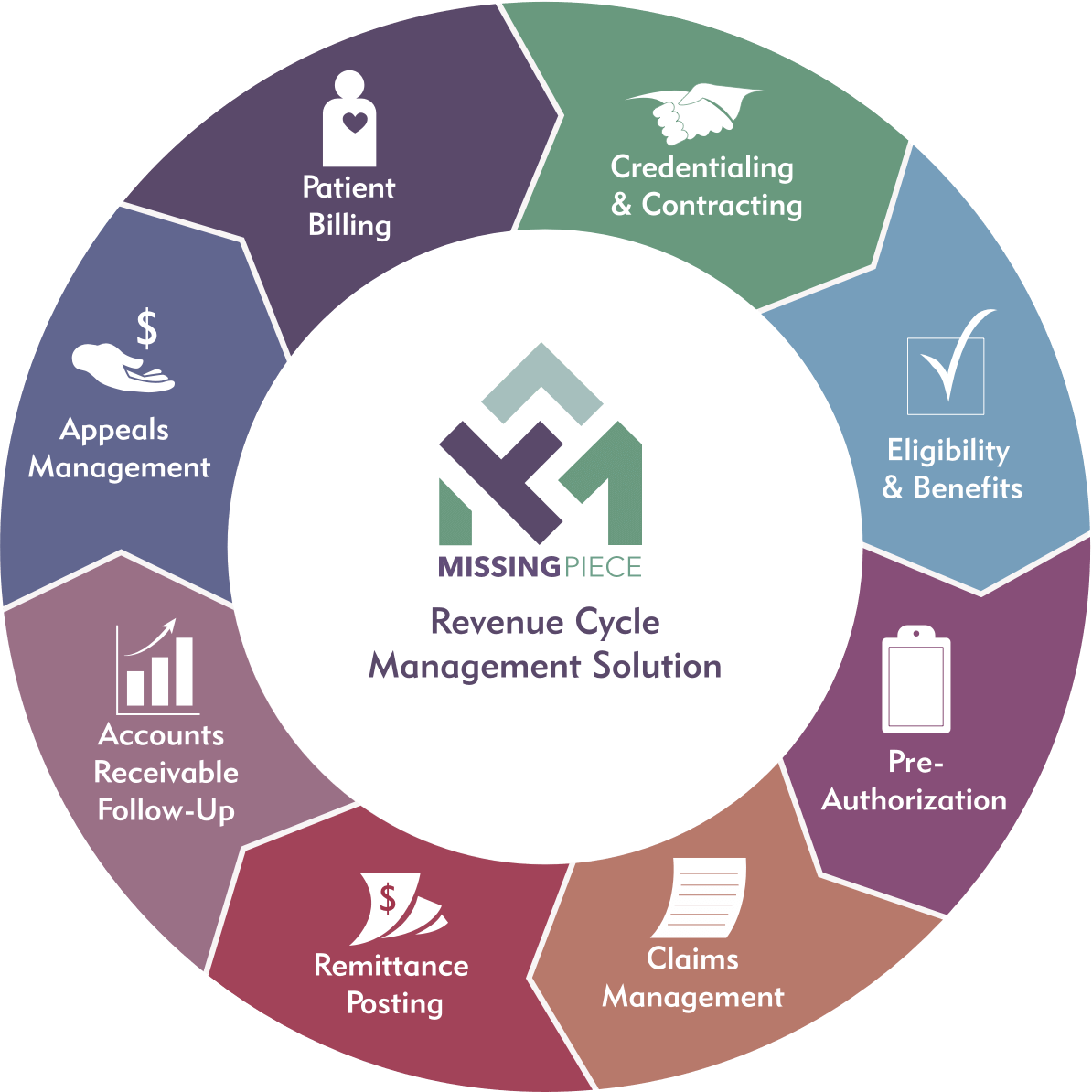
Missing Piece provides a comprehensive revenue cycle solution that manages every aspect of the occupational therapy billing and collection process for you. If your practice is just getting started, our industry experts will guide you on best practices to maximize your revenue. If you are an established practice looking to take your business to the next level, outsourcing billing services and partnering with an expert relieve you of the administrative burden of billing so you can focus on growing your practice. No matter what stage you are in, our team is here to help so you can focus on what’s important — providing the highest quality patient care.
Implementation
We understand implementing a new Revenue Cycle Management (RCM) solution can be overwhelming. Through our years of industry experience, ABA expertise, and unique onboarding processes, our team will lead you through a smooth and easy transition.
We analyze your existing payer contracts and ensure fee schedules and payer enrollments are correctly set up. Additionally, we verify benefits for each of your patients and complete outstanding authorizations. Your billing preferences are configured into our system and documented as standard operating procedures. The Implementation Team ensures all processes are running smoothly before transitioning management of your account to our Operations Team. Our practice management software makes the day-to-day management of ABA insurance billing services easier and more accurate. Together, we can seamlessly transition into a lasting partnership.
Credentialing & Contracting
The foundation of a strong revenue cycle process begins with the credentialing and contracting of your billing clinicians. Our Contracting Team’s strong payer relationships, combined with their knowledge of the most up-to-date payer requirements, allow you to achieve maximum reimbursement. From submitting required provider profile information to securing accurate discipline contracts, we facilitate the entire process for you.
The Contracting Team provides ongoing management by maintaining your providers’ payer profiles, keeping track of re-credentialing requirements, administering regular contracting updates, and ensuring ERA/EFT remain current to ensure payments are correctly assigned.
Eligibility & Benefits
We understand that navigating patient benefits is both challenging and time-consuming. Inaccurate eligibility and benefit quotes can be costly. Our Eligibility Team helps you mitigate the risk by performing comprehensive eligibility verifications. With our experts at the helm, you don’t need to worry about what to include in the ABA intake paperwork or any of the other daily time-consuming administrative tasks.
Communicating benefit information to patients is important. If you prefer, we will discuss with your patients any financial obligations they can expect, such as deductibles, copays, and out-of-pocket maximums, so you can focus on providing clinical care.
Pre-Authorization
Almost all payers require authorization before services are rendered. An important aspect of this requirement is demonstrating medical necessity. Our team of Authorization specialists, made up of expert medical billing consultants, understands payer medical necessity requirements and works to obtain authorization for the full recommended treatment.
Authorization specialists provide the following ongoing services:
- Managing appeals for authorization denials
- Keep your providers updated with payer-specific treatment plan guidelines for reimbursement.
- Tracking authorization usage and expiration dates, and obtaining timely re-authorization.
- Obtaining authorizations for assessments, ongoing treatment, and re-authorizations for ABA Therapy, speech, occupational and physical therapy.
Claims Management
Timely reimbursement requires that claims satisfy payer billing guidelines. Our team of Billing Specialists ensures claims meet payer-specific guidelines. Our claims processing system maintains up-to-date edits to prevent claim rejections and proactively monitors claim acceptance and processing. Our experts have all of the essential information on hand, such as the latest billing codes for occupational therapy claims. Our goal is to minimize the time from when the claim is submitted to when you receive payment.
Remittance Posting
Shortening the revenue cycle requires proactive monitoring. By maximizing electronic payments, we eliminate paper and receive electronic remittance advices (ERAs) and electronic fund transfers (EFTs) to automate remittance posting. This enables us to proactively pursue full reimbursement and investigate exceptions such as non-contractual adjustments, unexpected patient balances, and underpayments. Our Remittance Team’s expertise in understanding payer fee schedules and confusing adjustment codes ensures that improper adjustments and denials are pursued so you receive reimbursement according to your contracts.
Accounts Receivable Follow-up
Our Accounts Receivable team’s payer intelligence enables us to successfully obtain full reimbursement for ABA insurance billing and other services billed. At the core of our Revenue Cycle Management Solution is our Accounts Receivable team of billing experts who serve as advocates for you and your patients. This hands-on approach allows ABA providers to collect revenue they might otherwise miss or simply not have the resources to pursue.
Appeals Management
An appeal may be necessary when an authorization request or a claim is denied in full or in part. Typically, these appeals would require medical necessity rationale to support services. Our team of specialists will determine the payer’s appeal policy and guide you accordingly. Our appeal experience and ABA medical necessity knowledge enable us to successfully overturn denials and collect payments that rightfully belong to you. Successful appeal management is one of the top benefits of outsourcing ABA billing. It means you can continue providing quality services to your patients while we fight the battles with payers for your revenue.
Patient Billing
As patients bear more financial responsibility for healthcare costs, patient billing has become an important part of the revenue cycle. Compassion for the patient and family may seem at odds with optimizing reimbursement. Our RCM solution combines a robust process, flexible policies, and technology that provides a convenient and personalized approach to payment that meets both objectives.
When you outsource medical billing to us, you can rest assured that we combine best practices with your policies in designing your patient billing process and patient communication protocols. This ensures a positive patient experience that goes above and beyond what you would expect from a billing partner. We offer customized patient statements by mail and email, an online payment portal, and payment plans based on the patient’s financial circumstances, providing you the tools to offer flexible billing options while meeting your revenue cycle goals.
